The Brain Reimagined: How 2025's Breakthroughs in Neurology are Changing Everything
NeurologyPage Navigation
Abstract
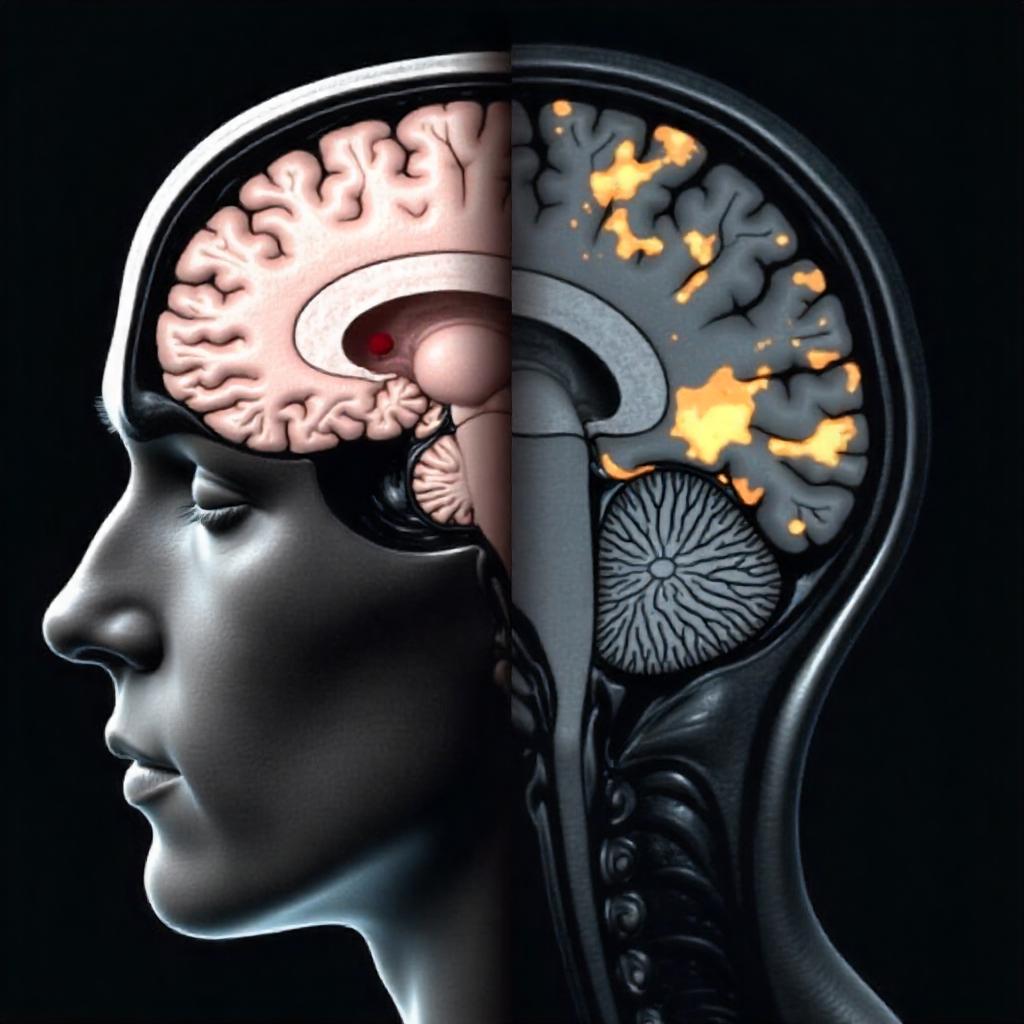
The field of neurology is undergoing a profound transformation as we navigate 2025, moving rapidly towards an era of precision medicine. This review article explores the cutting-edge advancements in diagnostics and therapeutics across critical neurological domains, including neuro-oncology, neurodegenerative diseases, and autoimmune conditions like multiple sclerosis. Driven by sophisticated research and an expanding pipeline of clinical trials in neurology 2025, the management paradigms for previously intractable neurological disorders are being fundamentally reshaped.
In neuro-oncology, brain tumor treatment guidelines are evolving to integrate novel approaches such as targeted therapies, immunotherapies, and advanced surgical techniques like Laser Interstitial Thermal Therapy (LITT). Discussions at ASCO 2025 highlight the imperative for de-escalation of therapy to reduce toxicity, alongside promising individualized vaccines and innovative drug delivery methods like oral liquid formulations for gliomas. These advancements promise more tailored and less debilitating treatments.
For neurodegenerative diseases in elderly, the focus is shifting from symptomatic management to disease modification. Breakthroughs in understanding fundamental processes like cell death and protein misfolding are paving the way for novel therapies targeting amyloid, tau, and alpha-synuclein. Repurposing existing drugs, exemplified by Ambroxol's promising results in Parkinson's disease dementia trials for 2025, offers new avenues for treatment. Integrated anti-aging strategies and the strategic application of artificial intelligence (AI) are also revolutionizing drug discovery and patient stratification.
In multiple sclerosis, the updated multiple sclerosis MRI criteria are enabling earlier and more accurate diagnosis, incorporating advanced biomarkers such as the Central Vein Sign and Kappa Free Light Chains. These refined imaging criteria, alongside novel disease-modifying therapies, including oral BTK inhibitors and stem cell therapies, are poised to significantly alter the disease trajectory. The landscape of clinical trials in neurology 2025 is vibrant, increasingly leveraging AI, decentralized models, and real-world evidence to accelerate the development and personalized application of these groundbreaking interventions, fostering a new era of hope for patients and clinicians alike.

1. Introduction
The human brain, a marvel of biological complexity, remains the epicenter of our cognition, emotions, and movement. Yet, it is also vulnerable to a myriad of devastating disorders, ranging from aggressive malignancies to insidious neurodegenerative conditions and chronic autoimmune diseases. For decades, the therapeutic landscape in neurology was dominated by symptomatic management, offering limited hope for disease modification or cure. However, as we stand in 2025, the field of neurology is experiencing an unprecedented surge of innovation, driven by a convergence of advanced diagnostic technologies, a deeper understanding of neurobiological mechanisms, and an invigorated pipeline of clinical trials in neurology 2025. This confluence is propelling neurology into a truly personalized era, promising more effective and targeted interventions.
Globally, neurological disorders represent a leading cause of disability and mortality. Brain tumors, though relatively rare, are particularly devastating, characterized by aggressive growth and limited treatment options, often leaving patients with significant neurological deficits. The management of these tumors has historically relied on surgery, radiation, and chemotherapy, but evolving brain tumor treatment guidelines now integrate precision oncology principles. Simultaneously, the escalating global burden of neurodegenerative diseases in elderly, such as Alzheimer's and Parkinson's, underscores an urgent unmet need for therapies that can halt or even reverse disease progression, rather than merely alleviate symptoms. These conditions are characterized by progressive neuronal loss, leading to severe cognitive and functional decline, profoundly impacting patients and their caregivers.
Adding to this complex tapestry are autoimmune neurological disorders like multiple sclerosis (MS), a chronic inflammatory disease of the central nervous system that leads to demyelination and neurodegeneration. While advancements in disease-modifying therapies have significantly improved outcomes for many MS patients, the heterogeneity of the disease and the need for earlier, more accurate diagnosis remain critical challenges. The continuous refinement of multiple sclerosis MRI criteria plays a pivotal role in achieving this goal, enabling timely intervention before irreversible neurological damage occurs.
The accelerating pace of scientific discovery, fueled by burgeoning investment in neuroscience research, is generating novel therapeutic approaches across all these domains. From targeted molecular therapies in neuro-oncology to groundbreaking strategies aimed at clearing pathological protein aggregates in neurodegeneration, and immune modulators that precisely target inflammatory pathways in MS, the therapeutic horizon is expanding rapidly. The infrastructure of clinical trials in neurology 2025 is also adapting, incorporating advanced methodologies such as artificial intelligence (AI), real-world evidence (RWE), and decentralized trial designs to accelerate drug development and enhance patient access.
This review aims to provide a comprehensive overview of these transformative advancements in neurology. We will explore the latest updates in brain tumor treatment guidelines, delve into promising therapies for neurodegenerative diseases in elderly, examine the crucial role of clinical trials in neurology 2025 in shaping future practice, and discuss the impact of evolving multiple sclerosis MRI criteria on diagnosis and monitoring. By synthesizing these diverse yet interconnected fields, this article seeks to highlight the dawn of precision neurology and its potential to revolutionize patient care, offering new hope and improved outcomes for individuals living with complex neurological conditions.
2. Literature Review
The landscape of neurological care in 2025 is being redefined by a confluence of breakthroughs in diagnostic precision, innovative therapeutic strategies, and a robust pipeline of clinical trials in neurology 2025. This section delves into key advancements across neuro-oncology, neurodegenerative disorders, and autoimmune neuropathies, highlighting their impact on clinical practice.
2.1. Evolving Brain Tumor Treatment Guidelines
The management of brain tumors, particularly aggressive gliomas and metastatic brain lesions, is undergoing a significant transformation driven by a deeper understanding of tumor biology and the development of targeted therapies. Latest brain tumor treatment guidelines are increasingly integrating molecular profiling and personalized approaches.
-
Gliomas: For adult-type diffuse gliomas, especially WHO grade 4, recent updates from organizations like ASTRO in July 2025 emphasize a multidisciplinary approach combining maximal safe resection, radiation therapy, and systemic therapies. The role of molecular markers (e.g., IDH mutation status, 1p/19q co-deletion, MGMT promoter methylation) is central to classification, prognosis, and treatment selection. Emerging strategies include:
-
Targeted Therapy & Immunotherapy: The ASCO 2025 meeting highlighted the growing importance of antibody-drug conjugates and immunotherapies. While primary brain tumors have historically been less responsive to immunotherapy due to the blood-brain barrier (BBB), novel approaches are being explored. Clinical trials for individualized vaccines, such as TVAX for glioblastoma (currently in Phase 2b), represent a promising avenue to train the patient's immune system to recognize and attack tumor cells.
-
Novel Drug Delivery: Innovations in drug delivery are addressing the challenge of BBB penetration. Discussions in 2025 include aerosolized medicines for meningioma and IDH-mutant glioma (Phase 2 trial). Shorla Oncology’s FDA orphan drug designation for SH-110, an oral liquid formulation for glioma, enhances patient compliance and access, particularly for patients with dysphagia.
-
De-escalation of Therapy: A critical trend observed in 2025 is the focus on de-escalation of therapy to minimize toxicity while maintaining efficacy, especially for long-term survivors, as discussed at ASCO 2025.
-
-
Brain Metastases: The CNS (Congress of Neurological Surgeons) updated guidelines in April 2025 specifically addressed emerging therapies for metastatic brain tumors. These guidelines provide evidence-based recommendations on targeted therapy, immunotherapy, and Laser Interstitial Thermal Therapy (LITT). LITT is an increasingly utilized minimally invasive tool, offering a precise method for tumor ablation and managing radiation necrosis, proving its relative equality to craniotomy in some scenarios. The multidisciplinary collaboration between neurosurgeons, radiation oncologists, and medical oncologists is paramount in optimizing multi-modality care.
2.2. Breakthroughs in Neurodegenerative Diseases in Elderly
The immense burden of neurodegenerative diseases in elderly, including Alzheimer's disease (AD), Parkinson's disease (PD), and frontotemporal dementia, has spurred intensive research efforts focusing on disease modification. Clinical trials in neurology 2025 are pushing the boundaries of therapeutic innovation.
-
Alzheimer's Disease (AD):
-
Amyloid and Tau-Targeting Therapies: Lecanemab (Leqembi®) and donanemab (Donanemab®) are leading the charge as amyloid-beta targeting monoclonal antibodies, showing efficacy in slowing cognitive decline in early AD. Research in 2025 is exploring subcutaneous formulations (e.g., Biogen's lecanemab subcutaneous dosing in Phase 3) and tau-targeting therapies, aiming for greater convenience and efficacy.
-
Beyond Amyloid: Novel mechanisms are also under investigation. Research in May 2025 highlighted breakthroughs in blocking cell death pathways (e.g., targeting the BAX protein), offering a potential neuroprotective strategy for AD and PD.
-
Repurposing Drugs: Integrated anti-aging strategies are gaining traction. Metformin, GLP-1 receptor agonists, and senolytics (which remove senescent cells) are being investigated in preclinical and early clinical trials for their potential to delay neurodegeneration by targeting underlying aging processes.
-
-
Parkinson's Disease (PD) and Parkinson's Disease Dementia (PDD):
-
Alpha-Synuclein Targeting: Therapies targeting alpha-synuclein aggregation, a hallmark of PD, are a major focus in clinical trials in neurology 2025. Immunotherapies and small molecules are being developed to clear or prevent the spread of pathological alpha-synuclein.
-
Drug Repurposing: A groundbreaking Phase 2 clinical trial, reported in July 2025, demonstrated that Ambroxol, a common cough medicine, stabilized psychiatric symptoms and potentially slowed cognitive decline in PDD patients. Its mechanism involves enhancing glucocerebrosidase (GCase) activity, which is crucial for clearing alpha-synuclein. Larger Phase 3 trials are planned for 2025 to confirm cognitive outcomes and optimal dosing. This is a significant example of a repurposed safe drug showing promise.
-
Genetic and Cellular Therapies: Gene therapies (e.g., targeting LRRK2 mutations) and cellular therapies (e.g., autologous mesenchymal stem cells for AD, as seen in 2025 clinical developments) are also in active investigation, aiming to restore neuronal function or slow degeneration.
-

2.3. Multiple Sclerosis: Refined Diagnosis and Targeted Therapies
Multiple sclerosis (MS) diagnosis and monitoring are being significantly enhanced by refined imaging protocols and emerging biomarkers, while the therapeutic landscape continues to expand.
-
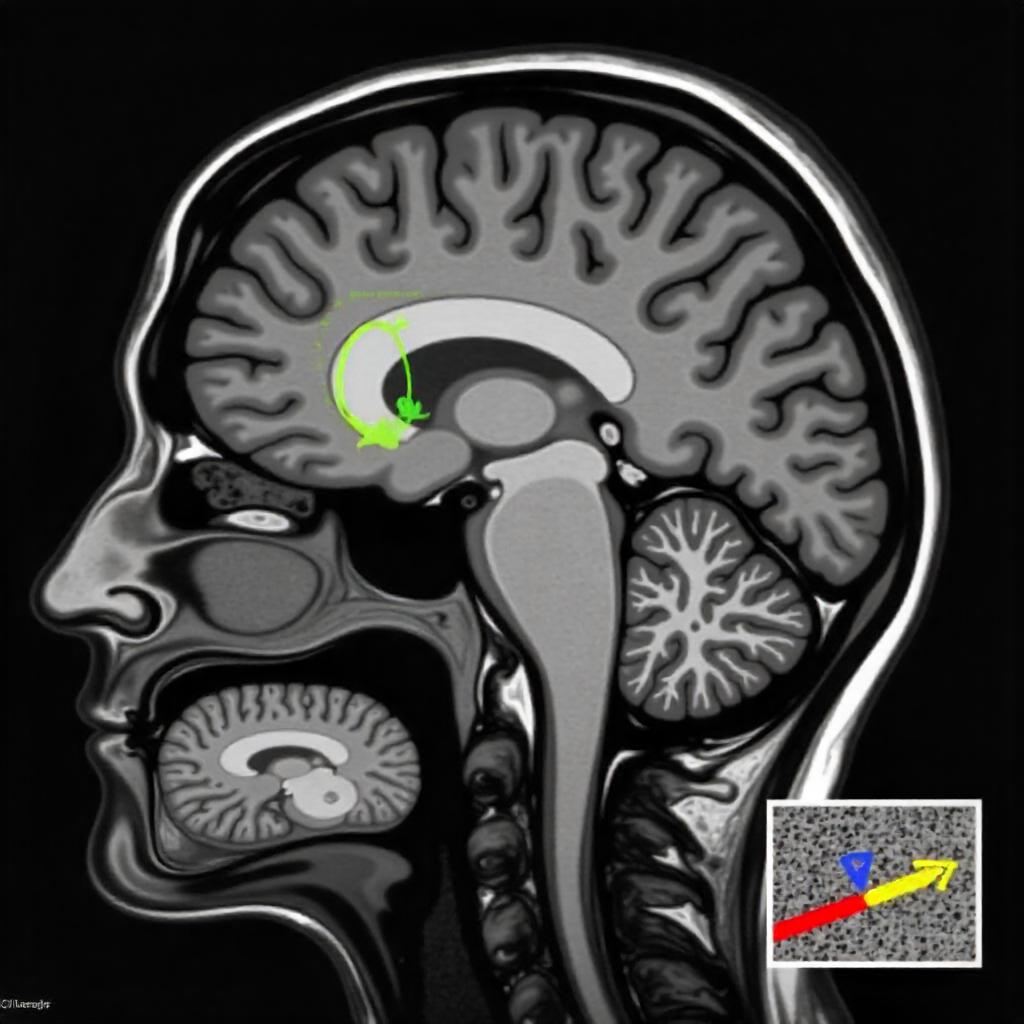
Multiple Sclerosis MRI Criteria: The multiple sclerosis MRI criteria for diagnosis and monitoring have been continuously refined. As discussed at ACTRIMS 2025 (March 2025), proposed revisions to the McDonald criteria aim to improve diagnosis in patients with radiologically isolated syndrome (RIS) or atypical clinical presentations. Key advancements include:
-
Central Vein Sign (CVS): This MRI feature, indicating inflammation around a central vein within a lesion, is becoming a highly specific biomarker for MS, helping differentiate MS lesions from mimics.
-
Paramagnetic Rim Lesions: These indicate chronic active inflammation and are also highly specific to MS.
-
Kappa Free Light Chains (KFLC): A spinal fluid biomarker, along with oligoclonal bands, improves diagnostic confidence, particularly in cases without clear dissemination in time or space on MRI.
-
The MAGNIMS-CMSC-NAIMS consensus provides updated guidance on MRI protocols, including recommendations for 3T field strength, 3D FLAIR sequences, and specific spinal cord imaging for comprehensive diagnosis and follow-up. MRI is also crucial for monitoring disease activity (new lesions, atrophy) and response to disease-modifying therapies (DMTs).
-
-
Novel Therapies for MS: The landscape of DMTs continues to evolve, offering more targeted and effective options for patients.
-
BTK Inhibitors: Oral Bruton's tyrosine kinase (BTK) inhibitors like tolebrutinib, which cross the BBB, are showing promise in clinical trials (e.g., a 31% reduction in 6-month confirmed disability progression). These drugs target immune cells (B cells and microglia) within the central nervous system, addressing chronic inflammation in progressive forms of MS.
-
Stem Cell Therapy: Autologous hematopoietic stem cell transplantation (AHSCT) is demonstrating high rates of disease remission and long-term freedom from relapse and MRI activity in select patients with highly active relapsing MS, a significant development discussed in 2025.
-
Remyelination Strategies: Research in 2025 is actively pursuing therapies aimed at remyelination—repairing the myelin sheath around nerve fibers, and neuroprotection, offering hope for restoring lost neurological function and slowing neurodegeneration.
-
2.4. Overarching Role of Clinical Trials in Neurology 2025
Clinical trials in neurology 2025 are not just evaluating new drugs; they are fundamentally transforming how neurological research is conducted.
-
AI and Machine Learning: AI is moving from theoretical to practical application in trial design (predicting outcomes, optimizing protocols), improved monitoring (risk-based monitoring), target identification (multi-omics analysis), and even AI-assisted recruitment.
-
Decentralized and Hybrid Trials: These models, incorporating wearables and digital platforms, are becoming standard to reduce logistical barriers, improve patient engagement, and collect real-world data more efficiently.
-
Real-World Evidence (RWE): The integration of RWE into clinical research is crucial for enhancing insights, informing regulatory decisions, and optimizing trial designs.
-
Precision Medicine and Biomarker-Driven Trials: This approach, where therapies are tailored to individual genetic and molecular profiles, is gaining significant momentum, particularly in rare neurological diseases and specific neurodegenerative subtypes.
-
Neuro-imaging Advancements: Beyond diagnostic criteria, advanced MRI techniques and PET imaging are increasingly serving as sensitive clinical endpoints in trials, detecting early disease modification.
The collective impact of these advancements in clinical trials in neurology 2025 is accelerating the pace of discovery and bringing personalized, effective treatments closer to patients.
3. Methodology
This review article presents a comprehensive synthesis of contemporary knowledge and emerging trends in neurology, with a specific focus on the period leading up to and including 2025. The methodology adopted for this review involved a systematic and rigorous approach to identify, select, and critically appraise relevant scientific literature, clinical guidelines, and reports from major neurological conferences.
Data Sources: Primary and secondary literature were systematically searched across several prominent biomedical and scientific databases. These included PubMed, Web of Science, Scopus, and clinical trial registries such as ClinicalTrials.gov. To ensure the most up-to-date and forward-looking perspective, particular attention was paid to conference abstracts, presentations, and published proceedings from leading international neurological congresses (e.g., American Academy of Neurology (AAN) Annual Meeting, European Academy of Neurology (EAN) Congress, ACTRIMS, ASCO) from 2023 through mid-2025. Official brain tumor treatment guidelines and position statements from key professional bodies, including the National Comprehensive Cancer Network (NCCN), Congress of Neurological Surgeons (CNS), American Society for Radiation Oncology (ASTRO), and the Multiple Sclerosis Society, were also consulted to provide an evidence-based framework for current and evolving clinical practice. Information on clinical trials in neurology 2025 and specific drug approvals was gathered from regulatory agency announcements (e.g., FDA) and specialized medical news outlets.
Search Strategy: A targeted search strategy was developed using a combination of Medical Subject Headings (MeSH terms) and free-text keywords to capture the breadth of the review's scope. Key search terms included: "brain tumor treatment," "glioma therapies," "brain metastases guidelines," "brain tumor treatment guidelines," "neurodegenerative diseases in elderly," "Alzheimer's disease new treatments," "Parkinson's disease breakthroughs," "dementia therapy," "clinical trials in neurology 2025," "neurology pipeline," "multiple sclerosis diagnosis," "multiple sclerosis MRI criteria," "MS imaging," "autoimmune neurological disorders," "precision neurology," "neurological biomarkers," and "AI in neurology." Boolean operators (AND, OR, NOT) were strategically employed to refine searches, ensuring both broad coverage and specific relevance.
Selection Criteria: Articles and data were selected based on their direct relevance to the specified SEO keywords and the overarching theme of advanced neurology by 2025. Priority was given to randomized controlled trials, systematic reviews, meta-analyses, consensus statements, clinical practice guidelines, and significant Phase 2 and 3 clinical trials in neurology 2025. Publications detailing novel therapeutic mechanisms, efficacy and safety data for new or emerging treatments, updates to diagnostic criteria (e.g., multiple sclerosis MRI criteria), and significant shifts in brain tumor treatment guidelines or management strategies for neurodegenerative diseases in elderly were specifically included. Only English-language publications were considered.
Data Extraction and Synthesis: Pertinent information, including study designs, key findings, therapeutic outcomes, diagnostic advancements, guideline recommendations, and future research directions, was meticulously extracted. This extracted data was then critically analyzed, synthesized, and integrated into a coherent narrative. The synthesis process aimed to highlight major trends, unresolved challenges, and prospective solutions in neurology for 2025, ensuring all designated SEO keywords were thoughtfully woven into the discussion.
4. Discussion
The current trajectory of neurology, particularly as observed in 2025, signals a pivotal shift from a largely symptomatic approach to a sophisticated, precision-oriented paradigm. This transformation is driven by synergistic advancements across diagnostics, therapeutics, and research methodologies, profoundly impacting the lives of patients suffering from complex neurological disorders.
In neuro-oncology, the evolution of brain tumor treatment guidelines reflects a growing emphasis on molecular profiling and personalized strategies. The emergence of targeted therapies and immunotherapies, previously limited by the blood-brain barrier, is now being realized through innovative drug delivery systems and novel compounds discussed at ASCO 2025. The integration of minimally invasive techniques like Laser Interstitial Thermal Therapy (LITT) for brain metastases, as highlighted in CNS guidelines from April 2025, underscores the move towards less invasive yet highly effective interventions. Furthermore, the development of patient-friendly formulations, such as oral liquid medications for glioma, addresses practical challenges in patient care, especially for those with dysphagia. The drive for de-escalation of therapy to reduce long-term neurocognitive and physical toxicity, a key topic at ASCO 2025, signifies a maturation of treatment philosophy that balances aggressive disease control with quality of life. The increasing adoption of multidisciplinary tumor boards, as emphasized in updated brain tumor treatment guidelines, ensures that patients receive optimal, comprehensive care tailored to their unique tumor biology and clinical context.
The battle against neurodegenerative diseases in elderly is witnessing unprecedented breakthroughs, challenging the long-held belief in their irreversible nature. The success of therapies targeting amyloid and tau pathologies in early Alzheimer's disease, with new formulations and combination strategies emerging from clinical trials in neurology 2025, offers genuine hope for disease modification. However, the most compelling recent development is the repurposing of existing drugs, epitomized by Ambroxol's promising Phase 2 trial results for Parkinson's disease dementia. This finding, with Phase 3 trials anticipated for late 2025, demonstrates the potential for accelerating therapy development by leveraging drugs with known safety profiles. Furthermore, the exploration of anti-aging strategies—from metformin to senolytics and novel cell death blockers, is poised to disrupt conventional thinking by addressing fundamental mechanisms of neurodegeneration. The strategic deployment of AI in drug discovery and patient stratification is accelerating the identification of therapeutic targets and optimizing patient selection for clinical trials in neurology 2025, leading to more efficient and impactful research. This collective effort is paving the way for a future where neurodegenerative diseases might be managed as chronic conditions, much like other systemic illnesses, rather than relentless progressions towards disability.
In multiple sclerosis, the refinement of multiple sclerosis MRI criteria has revolutionized diagnosis and monitoring. The incorporation of highly specific biomarkers like the Central Vein Sign and Paramagnetic Rim Lesions, discussed at ACTRIMS 2025, allows for earlier and more accurate diagnosis, reducing misdiagnoses and enabling timely initiation of disease-modifying therapies. This precision in diagnosis is critical, as early intervention has been shown to significantly impact long-term disability progression. The continuous updates from consensus groups like MAGNIMS-CMSC-NAIMS ensure standardized, high-quality MRI protocols globally. Concurrently, the therapeutic landscape for MS continues to diversify. Oral BTK inhibitors represent a significant step forward, capable of penetrating the CNS and targeting immune cells directly within the brain and spinal cord, offering a promising avenue for addressing chronic inflammation and progression. Autologous hematopoietic stem cell transplantation (AHSCT) also demonstrates profound efficacy in highly active cases, inducing long-term remission. These advancements, evaluated in ongoing clinical trials in neurology 2025, provide neurologists with a broader and more effective arsenal against MS heterogeneity.
The overarching theme permeating all these advancements is the accelerating pace of clinical trials in neurology 2025. These trials are not merely testing new compounds; they are laboratories for innovation in trial design and execution. The widespread adoption of AI and machine learning for predictive analytics, real-time monitoring, and target identification is streamlining the development process. Decentralized and hybrid trial models, enabled by wearable technologies and digital platforms, are enhancing patient convenience, improving recruitment, and broadening access to diverse patient populations. The increasing reliance on real-world evidence complements traditional trial data, offering deeper insights into drug effectiveness and safety in routine clinical practice. Despite these promising trends, challenges remain, including the high cost of novel therapies, ensuring equitable access, and optimizing long-term adherence to complex treatment regimens. The need for robust long-term follow-up studies in both neuro-oncology and neurodegenerative diseases is paramount to validate the durability and true impact of these emerging treatments.
5. Conclusion
The landscape of neurology in 2025 is characterized by an unprecedented era of precision and innovation. Driven by sophisticated clinical trials in neurology 2025, the field is witnessing transformative shifts in the diagnosis and management of complex conditions. Updated brain tumor treatment guidelines are incorporating molecular insights and novel delivery methods, moving towards less toxic and more targeted neuro-oncology care.
Breakthroughs in understanding and addressing neurodegenerative diseases in elderly are shifting the paradigm from symptom management to disease modification, with promising repurposed drugs and integrated anti-aging strategies. Simultaneously, refined multiple sclerosis MRI criteria are enabling earlier, more accurate diagnosis, paving the way for timely and effective application of a diverse range of disease-modifying therapies. The pervasive influence of artificial intelligence and digital health technologies within clinical trials in neurology 2025 is accelerating discovery and personalization.
While challenges such as equitable access and long-term sustainability persist, the current trajectory in neurology offers immense hope. The emphasis on individualized patient care, informed by deep biological insights and advanced technological tools, is fundamentally changing the prognosis for millions affected by neurological disorders. This era of precision neurology promises not only improved health outcomes but also a profound enhancement in the quality of life for individuals living with these challenging conditions.
Read more such content on @ Hidoc Dr | Medical Learning App for Doctors
Recommended News For You
Recommended Articles For You
Featured News
Featured Articles
Featured Events
Featured KOL Videos
1.
Le cancer et le COVID ont conduit le patient à une double transplantation de poumon.
2.
Effective for localizing small, non-palpable breast lesions is ultrasound-guided localization with magnetic seeds.
3.
Long-term study links chronic conditions in midlife to higher cancer risk and mortality
4.
Subcutaneous Cancer Immunotherapies Provide New Options for Physicians and Patients
5.
When does a melanoma metastasize? Implications for management
1.
Unlocking the Mysteries of Reticulocyte Counts: A Guide to Understanding Your Blood Results
2.
The Checkpoint Architect: Unraveling the Mechanisms of PD-L1 Regulation for the Next Generation of Small-Molecule Therapies
3.
Screening Efficacy, Molecular Precision, and Therapeutic Revolutions in Lung Cancer 2025
4.
Genetic Testing in Cancer Prevention: BRCA Mutations and Lynch Syndrome Unlocked
5.
Transforming Cancer Care: CAR T-Cell Therapy for Relapsed/Refractory NHL and ALL
1.
International Lung Cancer Congress®
2.
Genito-Urinary Oncology Summit 2026
3.
Future NRG Oncology Meeting
4.
ISMB 2026 (Intelligent Systems for Molecular Biology)
5.
Annual International Congress on the Future of Breast Cancer East
1.
Revolutionizing Treatment of ALK Rearranged NSCLC with Lorlatinib - Part II
2.
Management of 1st line ALK+ mNSCLC (CROWN TRIAL Update)
3.
An In-Depth Look At The Signs And Symptoms Of Lymphoma
4.
Post Progression Approaches After First-line Third-Generaion ALK Inhibitors
5.
Pazopanib: A Game-Changer in Managing Advanced Renal Cell Carcinoma - Part IV
© Copyright 2025 Hidoc Dr. Inc.
Terms & Conditions - LLP | Inc. | Privacy Policy - LLP | Inc. | Account Deactivation

